IncomeShield – Integrated Plan
Health Insurance CLAIMS
We are committed to keeping our claim process as swift and convenient as we can so you can focus fully on getting better.
What you need to know.
Integrated Shield Plan claims for COVID-19:
As our borders progressively reopen to permit international travel, MOH is allowing Singapore Citizens and PRs who travel out of Singapore to claim for inpatient COVID-19 treatment from MediShield Life and Integrated Shield Plans on or after 20 Oct 2020, should they experience onset of COVID-19 symptoms within 14 days of their return to Singapore.
An integrated plan means that you have IncomeShield protection on top of MediShield Life coverage.
Check your policy documents for coverage on the treatment you seek and the ward you are entitled to.
You must be treated in a hospital/medical institution that is found in the List of Medical Institutions Participating in MediShield Life Scheme.
All claims have to be submitted electronically by hospital/medical institution through the system set up by MOH.
The hospital or medical institution in which you are getting treatment must know that you are covered under IncomeShield.
Find out if your treatment is covered under your plan and get helpful information you need to file your claims here.
Additional information before you claim.
Forms that you must bring along for your treatment are:
1. Completed Medical Claims Authorisation Form (MCAF).
This can be obtained from the Ministry of Health website or from hospital staff.
2. Other forms specific to the hospital.
3. Hospital’s Admission Authorisation Form (Inpatient and Day Surgery only).
4. IncomeShield Letter of Guarantee, if any (Inpatient and Day Surgery only).
You can obtain a LOG by calling us at 6332 1133 or through the hospital staff if you are getting treatment in a restructured hospital.
Inpatient hospital treatment in Singapore [1]
You will be covered for daily ward and treatment charges, surgical benefits (including day surgery) and inpatient hospital treatments as listed in schedule of benefits. Please refer to policy conditions for more details.
Outpatient hospital treatment in Singapore [1]
You will be covered for:
Please refer to policy conditions for more details.
Pre- and post-hospitalisation treatment [1]
For Enhanced IncomeShield [2]:
For IncomeShield: Expenses have to be incurred in Singapore within 90 days from the hospitalisation or day surgery.
Treatment given before or after emergency overseas treatment is not covered.
Emergency overseas treatment [1]
You will only be covered for serious injuries or medical conditions which require immediate medical treatment in a hospital to prevent death or serious damage to health. Pre- and post-hospitalisation treatment given before or after emergency overseas treatment is not covered.
Coverage Information [1]
Find out if your treatment is covered under your plan and get helpful information you need to file your claims here. All claims submitted are subjected to review in accordance with the terms and conditions of the policies.
For inpatient and outpatient hospital treatment in Singapore
The claim will be reviewed and the final claim outcome and payment (if applicable) will be transmitted to the hospital. The hospital will send the final bill to the patient and will process refunds (if applicable).
For claims which require further clarification, we will need more time to process your claim. For such cases, we will keep you informed.
For pre- and post-hospitalisation treatment and Emergency overseas treatment
It usually takes 14 working days to process your claim once all documents are received.
For claims which require further clarification, we will need more time to process your claim. For such cases, we will keep you informed.
Required documents
The hospital or medical institution will send us your claim through electronic submission. We will then review your claim under Daily Cash Rider if applicable.
If your IncomeShield Outpatient hospital treatment (including Cancer Drug Treatment) / Inpatient hospital treatment / Day Surgery claim was confirmed by medical institution that the treatments could not be electronically submitted, please follow the below steps for claim submission.
If you have submitted a claim to other policies / insurers / your employers / any other third parties who may have reimbursed your bills, please submit the following documents:
Claim forms
Required documents
You can file your claims online if you meet the following criteria:
Please submit your claims via My Income portal after you have received our letter informing you that your claim for inpatient hospitalisation or day surgery or outpatient hospital treatment has been approved.
Alternatively, you may submit via our health insurance portal here.
Required documents
If you have submitted a claim to other policies / insurers / your employers / any other third parties who may have reimbursed your bills, please submit the following documents:
For foreigners
* All overseas documents must be certified as true copies by your lawyer or any Notary Public. If the documents are in foreign language, please provide a version officially translated to English by a certified translator/ interpreter. You will have to bear the costs of the translation services, if any.
Claim forms
Submit your documents via My Income portal
Information is correct as at 22 April 2024.
Your queries answered.
Policies that are on standard terms and have been inforced for at least a year from the start date or the reinstatement date; whichever is later, will be eligible.
The following are some instances where the IncomeShield LOG may not be issued:
- The estimated claimable amount falls within the policy deductible amount;
- There is an exclusion in the policy;
- There is an outstanding recovery amount due to Income;
- Treatments at private clinics, public hospital's short-stay wards, outpatient treatments and community hospitals;
- Overseas treatments;
- Treatments for excluded conditions such as pregnancy related treatments, cosmetic surgery, HIV infection or AIDS related, please refer to the policy contract for the a full list of exclusions.
Do note that Income reserves the right to limit or decline the issuance of the IncomeShield LOG, even if the eligibility criteria is met.
This is a facility provided to IncomeShield policyholders at major hospitals in Singapore. The IncomeShield Letter of Guarantee or LOG can be used to help with the upfront cash deposit required for hospitalisation or day surgery, subject to the acceptance of the Hospital.
An insured who is eligible for IncomeShield LOG receives treatment that is provided by a private specialist from IncomeShield's Panel or Extended Panel, can benefit from an IncomeShield LOG amount of up to $30,000; while it is up to $10,000 for treatment that is not provided by our Panel. For treatment that is provided by specialist from a public hospital, the IncomeShield LOG amount is up to $50,000.
The IncomeShield LOG is a facility intended to assist in the pre hospitalisation or pre surgery process; it is not an indicator of claim approval and neither is the issued amount an indicator of the claim amount. The filed IncomeShield claim, with details of the medical conditions and its treatments, will require a review by Income.
Restructured Hospitals/Medical Institutions
- Alexandra Hospital
- Admiralty Medical Centre
- Changi General Hospital
- Khoo Teck Puat Hospital
- KK Women's And Children's Hospital
- National Cancer Centre
- National Heart Centre Of Singapore
- National University Hospital
- Ng Teng Fong General Hospital
- Sengkang General Hospital
- Singapore General Hospital
- Singapore National Eye Centre
- Tan Tock Seng Hospital
Private Hospitals/Medical Institutions
- Farrer Park Hospital
- Gleneagles Hospital
- Mount Alvernia Hospital
- Mount Elizabeth Hospital
- Mount Elizabeth Novena Hospital
- Parkway East Hospital
- Raffles Hospital
- Thomson Medical Centre
The Hospital administrators will assist to make the request on your behalf. If successful, the IncomeShield LOG will be issued to the hospital on the same day.
The hospital reserves the right to collect a partial or a full deposit of the bill or accept the issued IncomeShield LOG only for the waiver of the initial deposit. Following are some other situations where a deposit will be required:
- The total of the IncomeShield LOG amount and the estimated CPF Medisave withdrawal amount is insufficient to cover the required deposit;
- The IncomeShield policy is unable to provide coverage for the hospitalisation or day surgery;
- Ineligible claims or ineligible items or medical services that are excluded and/or are not part of the treatment; please refer to the policy contract for details.
You may approach the participating hospitals' administrators for assistance, they will assist to request for the IncomeShield LOG on your behalf. In order to activate the IncomeShield LOG, you will need to accept the IncomeShield LOG terms, authorise the CPF Medisave withdrawal and sign the Medical Claims Authorisation Form (MCAF).
The deductible is the amount that you will need to pay first before any claim is payable.
You are encouraged to attend financial counselling for a better understanding on the costs involved for your upcoming hospitalisation stay and take note of your plan coverage in order to make an informed choice. You can contact your insurance adviser if you need further advice.
You can refer to the following table for your ward entitlement based on the plan type that you have purchased. This is to ensure that your policy coverage under your IncomeShield plan is better able to meet the expenses for your corresponding ward.
| Plan Type [1] | Ward Type | Corresponding Deductibles [2] |
| Enhanced IncomeShield Preferred | Standard room in Private Hospital, excluding suites | $3,500 |
| Enhanced IncomeShield Advantage | Restructured Hospital for Ward Class A | $3,500 |
| Enhanced IncomeShield Basic | Restructured Hospital for Ward Class B1 | $2,500 |
| Enhanced IncomeShield Enhanced C | Restructured Hospital for Ward Class B2 and below | $2,000 (Ward Class B2 or B2+) $1,500 (Ward Class C) |
Yes, you can choose to stay in ward class C and we will apply the deductible of ward class C to your claim. We will use the benefits of your Enhanced IncomeShield Basic plan to process the claimable amount.
For example:
You are covered under Enhanced IncomeShield Basic plan and stay in ward class C. The benefits used to process the claimable amount will be that of Enhanced IncomeShield Basic plan and the deductible applicable is $1,500.
Yes, you can. However, we will only pay the percentage of the reasonable expenses for necessary medical treatment using the pro-ration factor which applies to Enhanced IncomeShield Basic plan as specified in the schedule of benefits.
Yes, you can do so. You should note that if you stayed in a lower ward class (hence entitled to a lower deductible) for the first admission but choose to upgrade to a higher ward class on your second admission (within the same policy year), the difference of the two deductibles will apply for the second claim only.
| Claimable amount | Ward Class | Deductible applied | Co-insurance Applied | Net amount paid | |
| First Admission | $3000 | Ward Class C | $1,500 | $150 | $1,350 |
| Second Admission | $3,000 | Ward Class B2 | $500 ($2,000 - $1,500) | $250 | $2,250 |
| Third Admission | $3,000 | Ward Class B2 | $0 | $300 | $2,700 |
You can contact your insurance adviser or email your enquiry to healthcare@income.com.sg. Alternatively, you can call our customer service officers at 6332 1133.
For Medisave-approved integrated medical insurance plans, other insurers providing similar medical coverage are required to refund the amounts paid out under the individual's IncomeShield plan.
For Medisave-approved integrated medical insurance plans, the accredited hospitals/clinics will submit the claims electronically to the insurer via the MediClaim System after your hospital discharge. This is a seamless process where the electronic claim is initiated after you complete the claim form in the hospitals/clinics.
After Income settles your claim, and if you have other insurance cover, you can still submit the claim to your insurer for reimbursement or recovery back to your IncomeShield plan.
How does this help you?
1. You can get reimbursement for the expenses that are not covered by IncomeShield (provided these expenses are covered by your other H&S plan).
2. You will preserve the annual benefit limits of your IncomeShield for any future claimable events.
3. Your premiums for IncomeShield can be kept affordable in the long run.
Here’s an example of how this works:
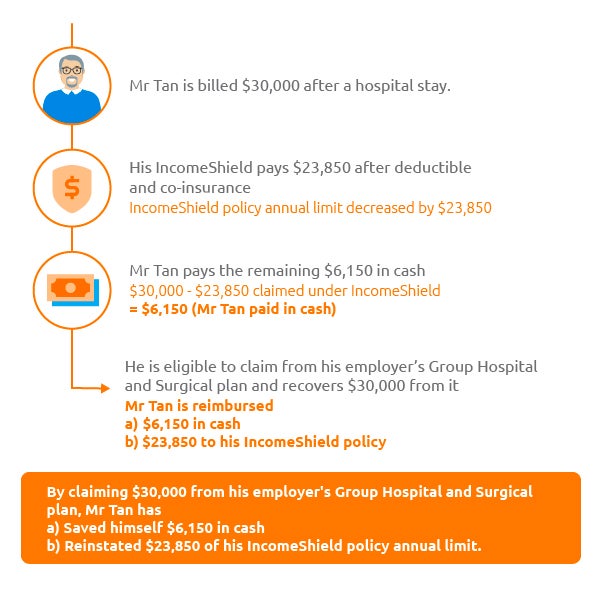
You can reach out to your Human Resource Department to understand the details of your employer’s medical insurance policy and its’ claim submission process.
Yes, you should claim from your personal insurance to enjoy the same benefits stated in FAQ Point 3. You may wish to approach your servicing agent or the insurer directly on the claim submission process.
How can you recover your claims from your employer?
STEP 1: Check with your company’s HR
Ask if you’re eligible for any Group Insurance coverage provided by your employer.
STEP 2: Submit documents to initiate a Group Insurance claim
Once HR confirms you’re eligible, submit the following documents to your company's HR or the respective company Group Insurance provider to initiate the refund:
Your company’s HR will liaise directly with the respective group insurer for the appropriate reimbursements into your IncomeShield plan. You won’t have to take any further action.
It is an insurance contract between your employer and/or other insurer(s) and yourself. While we are happy to assist you in the claim submission, we are unable to do so on your behalf as Income is not a party of your policy.
Yes, you will have to inform the hospital of your intention to claim from your employer and/or other insurer(s) first. For the unclaimed balance that you wish to claim under your IncomeShield plan, you will have to return to the hospital to submit the claim electronically via the MediClaim System. To facilitate with the submission request, you will need to bring along the settlement letter from your employer and/or other insurer(s). A copy of the said settlement letter should also be sent to us for review.
You may wish to take note that the submission will be done at the hospital’s discretion according to their internal practices and you may be charged an administrative fee. Therefore, we recommend you check the hospital’s submission procedures prior your hospitalisation, so that you can focus on your recovery without worrying about the claim administrative matters.
Get in touch with us.